A patient with suspected active tuberculosis is being transferred from a mental health facility to a medical center by emergency medical services. Which of the following should an infection preventionist recommend to the emergency medical technician (EMT)?
Place a surgical mask on both the patient and the EMT.
Place an N95 respirator on both the patient and the EMT.
Place an N95 respirator on the patient and a surgical mask on the EMT.
Place a surgical mask on the patient and an N95 respirator on the EMT.
Active tuberculosis (TB) is an airborne disease transmitted through the inhalation of droplet nuclei containing Mycobacterium tuberculosis. Effective infection control measures are critical during patient transport to protect healthcare workers, such as emergency medical technicians (EMTs), and to prevent community spread. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes the use of appropriate personal protective equipment (PPE) and source control as key strategies in the "Prevention and Control of Infectious Diseases" domain, aligning with guidelines from the Centers for Disease Control and Prevention (CDC).
For a patient with suspected active TB, the primary goal is to contain the infectious particles at the source (the patient) while ensuring the EMT is protected from inhalation exposure. Option C, placing an N95 respirator on the patient and a surgical mask on the EMT, is the most appropriate recommendation. The N95 respirator on the patient serves as source control by filtering the exhaled air, reducing the dispersion of infectious droplets. However, fitting an N95 respirator on the patient may be challenging, especially in an emergency setting or if the patient is uncooperative, so a surgical mask is often used as an alternative source control measure. For the EMT, a surgical mask provides a basic barrier but does not offer the same level of respiratory protection as an N95 respirator. The CDC recommends that healthcare workers, including EMTs, use an N95 respirator (or higher-level respiratory protection) when in close contact with a patient with suspected or confirmed active TB, unless an airborne infection isolation room is available, which is not feasible during transport.
Option A is incorrect because placing a surgical mask on both the patient and the EMT does not provide adequate respiratory protection for the EMT. Surgical masks are not designed to filter small airborne particles like those containing TB bacilli and do not meet the N95 standard required for airborne precautions. Option B is impractical and unnecessary, as placing an N95 respirator on both the patient and the EMT is overly restrictive and logistically challenging, especially for the patient during transport. Option D reverses the PPE roles, placing the surgical mask on the patient(insufficient for source control) and the N95 respirator on the EMT (appropriate for protection but misaligned with the need to control the patient’s exhalation). The CBIC and CDC guidelines prioritize source control on the patient and respiratory protection for the healthcare worker, making Option C the best fit.
This recommendation is consistent with the CBIC’s emphasis on implementing transmission-based precautions (CDC, 2005, Guideline for Preventing the Transmission of Mycobacterium tuberculosis in Healthcare Settings) and the use of PPE tailored to the mode of transmission, as outlined in the CBIC Practice Analysis (2022).
Which of the following activities will BEST prepare a newly hired infection preventionist to present information at the facility’s orientation program?
Observing other departments’ orientation presentations
Meeting with the facility’s leadership
Reviewing principles of adult learning
Administering tuberculin skin tests to orientees
The correct answer is C, "Reviewing principles of adult learning," as this activity will best prepare a newly hired infection preventionist to present information at the facility’s orientation program. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, effective education delivery, especially for healthcare professionals during orientation, relies on understanding adult learning principles (e.g., andragogy), which emphasize learner-centered approaches, relevance to practice, and active participation. Reviewing these principles equips the infection preventionist (IP) to design and deliver content that addresses the specific needs, experiences, and motivations of the audience—such as new staff learning infection control protocols—enhancing engagement and retention (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.1 - Develop and implement educational programs). This preparation ensures the presentation is tailored, impactful, and aligned with the goal of promoting infection prevention behaviors.
Option A (observing other departments’ orientation presentations) can provide insights into presentation styles or facility norms, but it is less focused on the IP’s specific educational role and may not address the unique content of infection prevention. Option B (meeting with the facility’s leadership) is valuable for understanding organizational priorities and gaining support, but it is more about collaboration and context-setting rather than direct preparation for presenting educational material. Option D (administering tuberculin skin tests to orientees) is a clinical task related to TB screening, not a preparatory activity for designing or delivering an educational presentation.
The focus on reviewing adult learning principles aligns with CBIC’s emphasis on evidence-based education strategies to improve infection control practices among healthcare personnel (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs). This approach enables the IP to effectively communicate critical information, such as hand hygiene or isolation protocols, during the orientation program.
Which of the following statements is true in considering work reassignment for pregnant employees?
Pregnant employees rarely require work reassignments
Pregnant employees who are positive for hepatitis B surface antibody may not care for hepatitis B patients
Pregnant employees should not be assigned to patients with known infections
Pregnant employees who are not immune to varicella should be excluded from pediatrics
Pregnant healthcare workerswho are not immune to varicella (chickenpox)are atincreased risk for severe complicationsif infected. These employees should be excluded from areas like pediatrics where exposure risk is elevated.
TheAPIC Textspecifies:
“Healthcare personnel who are not immune to varicella should avoid exposure to patients with active disease. In high-risk areas such as pediatrics, nonimmune pregnant employees should be reassigned”.
TheCIC Study Guidealso supports work exclusion or reassignment of nonimmune pregnant staff who have had exposure to varicella or are at risk.
Explanation of incorrect options:
A. Pregnant employees rarely require reassignment– False; reassignment is required in specific high-risk scenarios.
B. Hepatitis B surface antibody positivitymeans the employee is immune and can care for HBV patients.
C. Broad exclusion from all infected patientsis unnecessary and impractical.
A hospital experiencing an increase in catheter-associated urinary tract infections (CAUTI)implements a quality improvement initiative. Which of the following interventions is MOST effective in reducing CAUTI rates?
Routine urine cultures for all catheterized patients every 48 hours.
Implementing nurse-driven protocols for early catheter removal.
Replacing indwelling urinary catheters with condom catheters for all male patients.
Using antibiotic-coated catheters in all ICU patients.
Nurse-driven catheter removal protocols have been shown to significantly reduce CAUTI rates by minimizing unnecessary catheter use.
Routine urine cultures (A) lead to overtreatment of asymptomatic bacteriuria.
Condom catheters (C) are helpful in certain cases but are not universally effective.
Antibiotic-coated catheters (D) have mixed evidence regarding their effectiveness.
CBIC Infection Control References:
APIC Text, "CAUTI Prevention Strategies," Chapter 10.
An HBsAb-negative employee has a percutaneous exposure to blood from a Hepatitis B surface antigen (HBsAg) positive patient. Which of the following regimens is recommended for this employee?
Immune serum globulin and hepatitis B vaccine
Hepatitis B immune globulin (HBIG) alone
Hepatitis B vaccine alone
Hepatitis B immune globulin (HBIG) and hepatitis B vaccine
The correct answer is D, "Hepatitis B immune globulin (HBIG) and hepatitis B vaccine," as this is the recommended regimen for an HBsAb-negative employee with a percutaneous exposure to blood from an HBsAg-positive patient. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, which align with recommendations from the Centers for Disease Control and Prevention (CDC) and the Advisory Committee on Immunization Practices (ACIP), post-exposure prophylaxis (PEP) for hepatitis B virus (HBV) exposure depends on the employee’s vaccination status and the source’s HBsAg status. For an unvaccinated or known HBsAb-negative individual (indicating no immunity) exposed to HBsAg-positive blood, the standard PEP includes both HBIG and the hepatitis B vaccine. HBIG provides immediate passive immunity by delivering pre-formed antibodies, while the vaccine initiates active immunity to prevent future infections (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.2 - Implement measures to prevent transmission of infectious agents). The HBIG should be administered within 24 hours of exposure (preferably within 7 days), and the first dose of the vaccine should be given concurrently, followed by the complete vaccine series.
Option A (immune serum globulin and hepatitis B vaccine) is incorrect because immune serum globulin (ISG) is a general immunoglobulin preparation and not specific for HBV; HBIG, which contains high titers of anti-HBs, is the appropriate specific immunoglobulin for HBV exposure. Option B (hepatitis B immune globulin [HBIG] alone) is insufficient, as it provides only temporary passive immunity without initiating long-term active immunity through vaccination, which is critical for an unvaccinated individual. Option C (hepatitis B vaccine alone) is inadequate for immediate post-exposure protection, as it takes weeks to develop immunity, leaving the employee vulnerable in the interim.
The recommendation for HBIG and hepatitis B vaccine aligns with CBIC’s emphasis on evidence-based post-exposure management to prevent HBV transmission in healthcare settings (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.1 - Collaborate with organizational leaders). This dual approach is supported by CDC guidelines, which prioritize rapid intervention to reduce the risk of seroconversion following percutaneous exposure (CDC Updated U.S. Public Health Service Guidelines for the Management ofOccupational Exposures to HBV, HCV, and HIV, 2013).
Which of the following pathogens is associated with the highest risk of seroconversion after percutaneous exposure?
Shigella
Syphilis
Hepatitis A
Hepatitis C
Among the listed pathogens,Hepatitis Chas thehighest risk of seroconversion following a percutaneous exposure, though it's important to note thatHepatitis Bactually has the highest overall risk. However, since Hepatitis B is not listed among the options, the correct choice from the available ones isHepatitis C.
TheAPIC Textconfirms:
“The average risk of seroconversion after a percutaneous injury involving blood infected with hepatitis C virus is approximately 1.8 percent”.
The other options are not bloodborne pathogens typically associated with high seroconversion risks after needlestick or percutaneous exposure:
A. Shigella– transmitted fecal-orally, not percutaneously.
B. Syphilis– transmitted sexually or via mucous membranes.
C. Hepatitis A– primarily fecal-oral transmission, low occupational seroconversion risk.
During the past week, three out of four blood cultures from a febrile neonate in an intensive care unit grew coagulase-negative staphylococci. This MOST likely indicates:
Laboratory error.
Contamination.
Colonization.
Infection.
The scenario involves a febrile neonate in an intensive care unit (ICU) with three out of four blood cultures growing coagulase-negative staphylococci (CoNS) over the past week. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes accurate interpretation of microbiological data in the "Identification of Infectious Disease Processes" domain, aligning with the Centers for Disease Control and Prevention (CDC) guidelines for healthcare-associated infections. Determining whether this represents a true infection, contamination, colonization, or laboratory error requires evaluating the clinical and microbiological context.
Option B, "Contamination," is the most likely indication. Coagulase-negative staphylococci, such as Staphylococcus epidermidis, are common skin flora and frequent contaminants in blood cultures, especially in neonates where skin preparation or sampling technique may be challenging. The CDC’s "Guidelines for the Prevention of Intravascular Catheter-Related Infections" (2017) and the Clinical and Laboratory Standards Institute (CLSI) note that multiple positive cultures (e.g., two ormore) are typically required to confirm true bacteremia, particularly with CoNS, unless accompanied by clear clinical signs of infection (e.g., worsening fever, hemodynamic instability) and no other explanation. The inconsistency (three out of four cultures) and the neonate’s ICU setting—where contamination from skin or catheter hubs is common—suggest that the positive cultures likely result from contamination during blood draw rather than true infection. Studies, such as those in the Journal of Clinical Microbiology (e.g., Beekmann et al., 2005), indicate that CoNS in blood cultures is contaminated in 70-80% of cases when not supported by robust clinical correlation.
Option A, "Laboratory error," is possible but less likely as the primary explanation. Laboratory errors (e.g., mislabeling or processing mistakes) could occur, but the repeated growth in three of four cultures suggests a consistent finding rather than a random error, making contamination a more plausible cause. Option C, "Colonization," refers to the presence of microorganisms on or in the body without invasion or immune response. While CoNS can colonize the skin or catheter sites, colonization does not typically result in positive blood cultures unless there is an invasive process, which is not supported by the data here. Option D, "Infection," is the least likely without additional evidence. True CoNS bloodstream infections (e.g., catheter-related) in neonates are serious but require consistent positive cultures, clinical deterioration (e.g., persistent fever, leukocytosis), and often imaging or catheter removal confirmation. The febrile state alone, with inconsistent culture results, does not meet the CDC’s criteria for diagnosing infection (e.g., at least two positive cultures from separate draws).
The CBIC Practice Analysis (2022) and CDC guidelines stress differentiating contamination from infection to avoid unnecessary treatment, which can drive antibiotic resistance. Given the high likelihood of contamination with CoNS in this context, Option B is the most accurate answer.
What rate is expressed by the number of patients who acquire infections over a specified time period divided by the population at risk of acquiring an infection during that time period?
Incidence rate
Disease specific
Point prevalence
Period prevalence
Theincidence ratemeasuresnew cases of infection in a population over a defined time periodusing the formula:
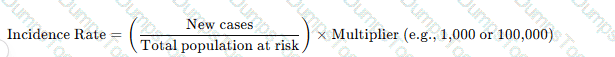
Why the Other Options Are Incorrect?
B. Disease specific– Refers to infectionscaused by a particular pathogen, not the general rate of new infections.
C. Point prevalence– Measuresexisting cases at a specific point in time, not new cases.
D. Period prevalence– Includesboth old and new cases over a set period, unlike incidence, which only considers new cases.
CBIC Infection Control Reference
APIC definesincidence rate as the number of new infections in a population over a given period.
Which of the following procedures has NOT been documented to contribute to the development of postoperative infections in clean surgical operations?
Prolonged preoperative hospital stay
Prolonged length of the operations
The use of iodophors for preoperative scrubs
Shaving the site on the day prior to surgery
Postoperative infections in clean surgical operations, defined by the Centers for Disease Control and Prevention (CDC) as uninfected operative wounds with no inflammation and no entry into sterile tracts (e.g., gastrointestinal or respiratory systems), are influenced by various perioperative factors. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes identifying and mitigating risk factors in the "Prevention and Control of Infectious Diseases" domain, aligning with CDC guidelines for surgical site infection (SSI) prevention. The question focuses on identifying a procedure not documented as a contributor to SSIs, requiring an evaluation of evidence-based risk factors.
Option C, "The use of iodophors for preoperative scrubs," has not been documented to contribute to the development of postoperative infections in clean surgical operations. Iodophors, such as povidone-iodine, are antiseptic agents used for preoperative skin preparation and surgical hand scrubs. The CDC’s "Guideline for Prevention of Surgical Site Infections" (1999) and its 2017 update endorse iodophors as an effective method for reducing microbial load on the skin, with no evidence suggesting they increase SSI risk when used appropriately. Studies, including those cited by the CDC, show that iodophors are comparable to chlorhexidine in efficacy for preoperative antisepsis, and their use is a standard, safe practice rather than a risk factor.
Option A, "Prolonged preoperative hospital stay," is a well-documented risk factor. Extended hospital stays prior to surgery increase exposure to healthcare-associated pathogens, raising the likelihood of colonization and subsequent SSI, as noted in CDC and surgical literature (e.g., Mangram et al., 1999). Option B, "Prolonged length of the operations," is also a recognized contributor. Longer surgical durations are associated with increased exposure time, potential breaches in sterile technique, and higher infection rates, supported by CDC data showing a correlation between operative time and SSI risk. Option D, "Shaving the site on the day prior to surgery," has been documented as a risk factor. Preoperative shaving, especially with razors, can cause microabrasions that serve as entry points for bacteria, increasing SSI rates. The CDCrecommends avoiding shaving or using clippers immediately before surgery to minimize this risk, with evidence from studies like those in the 1999 guideline showing higher infection rates with preoperative shaving.
The CBIC Practice Analysis (2022) and CDC guidelines focus on evidence-based practices, and the lack of documentation linking iodophor use to increased SSIs—coupled with its role as a preventive measure—makes Option C the correct answer. The other options are supported by extensive research as contributors to SSI development in clean surgeries.
The annual report for Infection Prevention shows a dramatic decrease in urinary catheter days, a decrease in the catheter utilization ratio, and a slight decrease in the number of catheter-associated urinary tract infections (CAUTIs). The report does not show an increase in the overall rate of CAUTI. How would the infection preventionist explain this to the administration?
The rate is incorrect and needs to be recalculated.
The rate may be higher if the denominator is very small.
The rate is not affected by the number of catheter days.
Decreasing catheter days will not have an effect on decreasing CAUTI.
The correct answer is B, "The rate may be higher if the denominator is very small," as this providesthe most plausible explanation for the observed data in the annual report. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, the CAUTI rate is calculated as the number of CAUTIs per 1,000 catheter days, where catheter days serve as the denominator. The report indicates a dramatic decrease in urinary catheter days and a slight decrease in the number of CAUTIs, yet the overall CAUTI rate has not increased. This discrepancy can occur if the denominator (catheter days) becomes very small, which can inflate or destabilize the rate, potentially masking an actual increase in the infection risk per catheter day (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.2 - Analyze surveillance data). A smaller denominator amplifies the impact of even a slight change in the number of infections, suggesting that the rate may be higher than expected or less reliable, necessitating further investigation.
Option A (the rate is incorrect and needs to be recalculated) assumes an error in the calculation without evidence, which is less specific than the denominator effect explanation. Option C (the rate is not affected by the number of catheter days) is incorrect because the CAUTI rate is directly influenced by the number of catheter days as the denominator; a decrease in catheter days should typically lower the rate if infections decrease proportionally, but the lack of an increase here suggests a calculation or interpretation issue. Option D (decreasing catheter days will not have an effect on decreasing CAUTI) contradicts evidence-based practice, as reducing catheter days is a proven strategy to lower CAUTI incidence, though the rate’s stability here indicates a potential statistical artifact.
The explanation focusing on the denominator aligns with CBIC’s emphasis on accurate surveillance and data analysis to guide infection prevention strategies, allowing the infection preventionist to advise administration on the need to review data trends or adjust monitoring methods (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.5 - Use data to guide infection prevention and control strategies). This insight can prompt a deeper analysis to ensure the CAUTI rate reflects true infection risk.
Healthcare workers are MOST likely to benefit from infection prevention education if the Infection Preventionist (IP)
brings in speakers who are recognized experts.
plans the educational program well ahead of time.
audits practices and identifies deficiencies.
involves the staff in determining the content.
The correct answer is D, "involves the staff in determining the content," as this approach is most likely to benefit healthcare workers from infection prevention education. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, effective education programs are tailored to the specific needs and contexts of the learners. Involving staff in determining the content ensures that the educational material addresses their real-world challenges, knowledge gaps, and interests, thereby increasing engagement, relevance, and application of the learned principles (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.1 - Develop and implement educational programs). This participatory approach fosters ownership and accountability among healthcare workers, enhancing the likelihood that they will adopt and sustain infection prevention practices.
Option A (brings in speakers who are recognized experts) can enhance credibility and provide high-quality information, but it does not guarantee that the content will meet the specific needs of the staff unless their input is considered. Option B (plans the educational program well ahead of time) is important for logistical success and preparedness, but without staff involvement, the program may lack relevance or fail to address immediate concerns. Option C (audits practices and identifies deficiencies) is a valuable step in identifying areas for improvement, but it is a diagnostic process rather than a direct educational strategy; education based solely on audits might not engage staff effectively if their input is not sought.
The focus on involving staff aligns with CBIC’s emphasis on adult learning principles, which highlight the importance of learner-centered education. By involving staff, the IP adheres to best practices for adult education, ensuring that the program is practical and tailored, ultimately leadingto better outcomes in infection prevention (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs). This approach also supports a collaborative culture, which is critical for sustaining infection control efforts in healthcare settings.
Documentation of each steam sterilization cycle should include which of the following pieces of information?
Load contents
Machine model number
Date sterilizer was cleaned
Initials of the person who prepared the instrument set
Documentation of each steam sterilization cycle is a regulatory and quality requirement. It must includeload contents, thesterilizer ID,date,cycle number, and theperson who assembled the load. These details support traceability and quality assurance.
TheAPIC Textstates:
“Each item or package should be labeled with a lot-control identifier that includes the sterilizer identification number or code, a detailed list of the contents, an identifier for the person who assembled the package, the date of sterilization, the cycle number...”
Other options like themachine model numberordate sterilizer was cleanedare not routine documentation elements for every cycle.
Which of the following factors increases a patient’s risk of developing ventilator-associated pneumonia (VAP)?
Hypoxia
Nasogastric tube
Acute lung disease
In-line suction
Ventilator-associated pneumonia (VAP) is a type of healthcare-associated pneumonia that occurs in patients receiving mechanical ventilation for more than 48 hours. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes identifying risk factors for VAP in the "Prevention and Control of Infectious Diseases" domain, aligning with the Centers for Disease Control and Prevention (CDC) guidelines for preventing ventilator-associated events. The question requires identifying which factor among the options increases a patient’s risk of developing VAP, based on evidence from clinical and epidemiological data.
Option B, "Nasogastric tube," is the correct answer. The presence of a nasogastric tube is a well-documented risk factor for VAP. This tube can facilitate the aspiration of oropharyngeal secretions or gastric contents into the lower respiratory tract, bypassing natural defense mechanisms like the epiglottis. The CDC’s "Guidelines for Preventing Healthcare-Associated Pneumonia" (2004) and studies in the American Journal of Respiratory and Critical Care Medicine (e.g., Kollef et al., 2005) highlight that nasogastric tubes increase VAP risk by promoting microaspiration, especially if improperly managed or if the patient has impaired gag reflexes. This mechanical disruption of the airway’s protective barriers is a direct contributor to infection.
Option A, "Hypoxia," refers to low oxygen levels in the blood, which can be a consequence of lung conditions or VAP but is not a primary risk factor for developing it. Hypoxia may indicate underlying respiratory compromise, but it does not directly increase the likelihood of VAP unless associated with other factors (e.g., prolonged ventilation). Option C, "Acute lung disease," is a broad term that could include conditions like acute respiratory distress syndrome (ARDS), which may predispose patients to VAP due to prolonged ventilation needs. However, acute lung disease itself is not a specific risk factor; rather, it is the need for mechanical ventilation that elevates risk, making this less direct than the nasogastric tube effect. Option D, "In-line suction," involves a closed-system method for clearing respiratory secretions, which is designed to reduce VAP risk by minimizing contamination during suctioning. The CDC and evidence-based guidelines (e.g., American Thoracic Society, 2016) recommend in-line suction to prevent infection, suggesting it decreases rather than increases VAP risk.
The CBIC Practice Analysis (2022) and CDC guidelines prioritize identifying modifiable risk factors like nasogastric tubes for targeted prevention strategies (e.g., elevating the head of the bed to reduce aspiration). Option B stands out as the factor most consistently linked to increased VAP risk based on clinical evidence.
What inflammatory reaction may occur in the eye after cataract surgery due to a breach in disinfection and sterilization of intraocular surgical instruments?
Endophthalmitis
Bacterial conjunctivitis
Toxic Anterior Segment Syndrome
Toxic Posterior Segment Syndrome
The correct answer is C, "Toxic Anterior Segment Syndrome," as this is the inflammatory reaction that may occur in the eye after cataract surgery due to a breach in disinfection and sterilization of intraocular surgical instruments. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, Toxic Anterior Segment Syndrome (TASS) is a sterile, acute inflammatory reaction that can result from contaminants introduced during intraocular surgery, such as endotoxins, residues from improper cleaning, or chemical agents left on surgical instruments due to inadequate disinfection or sterilization processes (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.3 - Ensure safe reprocessing of medical equipment). TASS typically presents within 12-48 hours post-surgery with symptoms like pain, redness, and anterior chamber inflammation, and it is distinct from infectious causes because it is not microbial in origin. A breach in reprocessing protocols, such as failure to remove detergents or improper sterilization, is a known risk factor, making it highly relevant to infection prevention efforts in surgical settings.
Option A (endophthalmitis) is an infectious inflammation of the internal eye structures, often caused by bacterial or fungal contamination, which can also result from poor sterilization but is distinguished from TASS by its infectious nature and longer onset (days to weeks). Option B (bacterial conjunctivitis) affects the conjunctiva and is typically a surface infection unrelated to intraocular surgery or sterilization breaches of surgical instruments. Option D (toxic posterior segment syndrome) is not a recognized clinical entity in the context of cataract surgery; inflammation in the posterior segment is more commonly associated with infectious endophthalmitis or other conditions, not specifically linked to reprocessing failures.
The focus on TASS aligns with CBIC’s emphasis on ensuring safe reprocessing to prevent adverse outcomes in surgical patients, highlighting the need for rigorous infection control measures (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.5 - Evaluate the environment for infection risks). This is supported by CDC and American Academy of Ophthalmology guidelines, which identify TASS as a preventable complication linked to reprocessing errors (CDC Guidelines for Disinfection and Sterilization, 2019; AAO TASS Task Force Report, 2017).
Which of the following factors should be considered when evaluating countertop surface materials?
Durability
Sink design
Accessibility
Faucet placement
The correct answer is A, "Durability," as it is a critical factor to consider when evaluating countertop surface materials. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, the selection of materials in healthcare settings, including countertop surfaces, must prioritize infection prevention and control. Durability ensures that the surface can withstand frequent cleaning, disinfection, and physical wear without degrading, which is essential to maintain a hygienic environment and prevent the harboring of pathogens (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.4 - Implement environmental cleaning and disinfection protocols). Durable materials, such as solid surface composites or stainless steel, resist scratches, cracks, and moisture damage, reducing the risk of microbial growth and cross-contamination, which are significant concerns in healthcare facilities.
Option B (sink design) relates more to the plumbing and fixture layout rather than the inherent properties of the countertop material itself. While sink placement and design are important for workflow and hygiene, they are secondary to the material's characteristics. Option C (accessibility) is a consideration for user convenience and compliance with the Americans with Disabilities Act (ADA), but it pertains more to the installation and layout rather than the material's suitability for infection control. Option D (faucet placement) affects usability and water management but is not a direct attribute of the countertop material.
The emphasis on durability aligns with CBIC’s focus on creating environments that support effective cleaning and disinfection practices, which are vital for preventing healthcare-associated infections (HAIs). Selecting durable materials helps ensure long-term infection prevention efficacy, making it a primary factor in the evaluation process (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.5 - Evaluate the environment for infection risks).
What question would be appropriate for an infection preventionist to ask when reviewing the discussion section of an original article?
Was the correct sample size and analysis method chosen?
Could alternative explanations account for the observed results?
Is the study question important, appropriate, and stated clearly?
Are criteria used to measure the exposure and the outcome explicit?
When reviewing the discussion section of an original article, an infection preventionist must focus on critically evaluating the interpretation of the study findings, their relevance to infection control, and their implications for practice. The discussion section typically addresses the meaning of the results, compares them to existing literature, and considers limitations or alternative interpretations. The appropriate question should align with the purpose of this section and reflect the infection preventionist's need to assess the validity and applicability of the research. Let’s analyze each option:
A. Was the correct sample size and analysis method chosen?: This question pertains to the methodology section of a research article, where the study design, sample size, and statistical methods are detailed. While these elements are critical for assessing the study's rigor, they are not the primary focus of the discussion section, which interprets results rather than re-evaluating the study design. An infection preventionist might ask this during a review of the methods section, but it is less relevant here.
B. Could alternative explanations account for the observed results?: The discussion section often explores whether the findings can be explained by factors other than the hypothesized cause, such as confounding variables, bias, or chance. This question is highly appropriate foran infection preventionist, as it encourages a critical assessment of whether the results truly support infection control interventions or if other factors (e.g., environmental conditions, patient factors) might be responsible. This aligns with CBIC's emphasis on evidence-based practice, where understanding the robustness of conclusions is key to applying research to infection prevention strategies.
C. Is the study question important, appropriate, and stated clearly?: This question relates to the introduction or background section of an article, where the research question and its significance are established. While important for overall study evaluation, it is not specific to the discussion section, which focuses on interpreting results rather than revisiting the initial question. An infection preventionist might consider this earlier in the review process, but it does not fit the context of the discussion section.
D. Are criteria used to measure the exposure and the outcome explicit?: This question is relevant to the methods section, where the definitions and measurement tools for exposures (e.g., a specific intervention) and outcomes (e.g., infection rates) are described. The discussion section may reference these criteria but focuses more on their implications rather than their clarity. This makes it less appropriate for the discussion section specifically.
The discussion section is where authors synthesize their findings, address limitations, and consider alternative explanations, making option B the most fitting. For an infection preventionist, evaluating alternative explanations is crucial to ensure that recommended practices (e.g., hand hygiene protocols or sterilization techniques) are based on solid evidence and not confounded by unaddressed variables. This critical thinking is consistent with CBIC's focus on applying research to improve infection control outcomes.
Which performance improvement model should the infection preventionist use to aid in the evaluation of the infection control plan?
Six Sigma
Failure mode and effects analysis
Plan, Do, Study, Act
Root Cause Analysis
ThePlan, Do, Study, Act (PDSA) modelis awidely used performance improvement tool in infection prevention. It focuses oncontinuous quality improvementthroughplanning, implementing, analyzing data, and making adjustments. This model aligns withinfection control program evaluationsandThe Joint Commission’s infection prevention and control standards.
Why the Other Options Are Incorrect?
A. Six Sigma– Adata-driven process improvement methodbut not as commonly used in infection control as PDSA.
B. Failure Mode and Effects Analysis (FMEA)– Used toidentify risks before implementation, rather than ongoing evaluation.
D. Root Cause Analysis (RCA)– Used toanalyze failures after they occur, rather than guiding continuous improvement.
CBIC Infection Control Reference
ThePDSA cycle is a recognized model for evaluating and improving infection control plans.
During the last week in June, an emergency department log reveals numerous cases of profuse watery diarrhea in individuals 74 years of age and older. During the same time period, four immunocompromised patients were admitted with possible Cryptosporidium. Which of the following actions should the infection preventionist take FIKST?
Characterize the outbreak by person, place, and time
Increase surveillance facility wide for additional cases
Contact the laboratory to confirm stool identification results
Form a tentative hypothesis about the potential reservoir for this outbreak
When an outbreak of infectious disease is suspected, the first step is to conduct an epidemiologic investigation. This begins withcharacterizing the outbreak by person, place, and timeto establish patterns and trends. This approach, known as descriptive epidemiology, provides critical insights into potential sources and transmission patterns.
Step-by-Step Justification:
Identify Cases and Patterns:
The infection preventionist should analyze patient demographics (person), locations of cases (place), and onset of symptoms (time). This helps in defining the outbreak scope and potential exposure sources.
Create an Epidemic Curve:
An epidemic curve helps determine whether the outbreak is a point-source or propagated event. This can indicate whether the infection is spreading person-to-person or originating from a common source.
Compare with Baseline Data:
Reviewing historical data ensures that the observed cases exceed the expected norm, confirming an outbreak.
Guide Further Investigation:
Establishing basic epidemiologic patterns guides subsequent actions, such as laboratory testing, environmental sampling, and surveillance.
Why Other Options Are Incorrect:
B. Increase surveillance facility-wide for additional cases:
While enhanced surveillance is important, it should follow the initial characterization of the outbreak. Surveillance without a defined case profile may lead to misclassification and misinterpretation.
C. Contact the laboratory to confirm stool identification results:
Confirming lab results is essential but comes after defining the outbreak's characteristics. Without an epidemiologic link, testing may yield results that are difficult to interpret.
D. Form a tentative hypothesis about the potential reservoir for this outbreak:
Hypothesis generation occurs after sufficient epidemiologic data have been collected. Jumping to conclusions without characterization may result in incorrect assumptions and ineffective control measures.
CBIC Infection Control References:
APIC Text, "Outbreak Investigations," Epidemiology, Surveillance, Performance, and Patient Safety Measures.
APIC/JCR Infection Prevention and Control Workbook, Chapter 4, Surveillance Program.
APIC Text, "Investigating Infectious Disease Outbreaks," Guidelines for Epidemic Curve Analysis.
Which of the following statements is true about the microbial activity of chlorhexidine soap?
As fast as alcohol
Can be used with any hand lotion
Poor against gram positive bacteria
Persistent activity with a broad spectrum effect
Chlorhexidine soap is a widely used antiseptic agent in healthcare settings for hand hygiene and skin preparation due to its effective antimicrobial properties. The Certification Board of Infection Control and Epidemiology (CBIC) underscores the importance of proper hand hygiene and antiseptic use in the "Prevention and Control of Infectious Diseases" domain, aligning with guidelines from the Centers for Disease Control and Prevention (CDC) and the World Health Organization (WHO). Understanding the microbial activity of chlorhexidine is essential for infection preventionists to recommend its appropriate use.
Option D, "Persistent activity with a broad spectrum effect," is the true statement. Chlorhexidine exhibits a broad spectrum of activity, meaning it is effective against a wide range of microorganisms, including gram-positive and gram-negative bacteria, some fungi, and certainviruses. Its persistent activity is a key feature, as it binds to the skin and provides a residual antimicrobial effect that continues to inhibit microbial growth for several hours after application. This residual effect is due to chlorhexidine’s ability to adhere to the skin’s outer layers, releasing slowly over time, which enhances its efficacy in preventing healthcare-associated infections (HAIs). The CDC’s "Guideline for Hand Hygiene in Healthcare Settings" (2002) and WHO’s "Guidelines on Hand Hygiene in Health Care" (2009) highlight chlorhexidine’s prolonged action as a significant advantage over other agents like alcohol.
Option A, "As fast as alcohol," is incorrect. Alcohol (e.g., 60-70% isopropyl or ethyl alcohol) acts rapidly by denaturing proteins and disrupting microbial cell membranes, providing immediate kill rates within seconds. Chlorhexidine, while effective, has a slower onset of action, requiring contact times of 15-30 seconds or more to achieve optimal microbial reduction. Its strength lies in persistence rather than speed. Option B, "Can be used with any hand lotion," is false. Chlorhexidine’s activity can be diminished or inactivated by certain hand lotions or creams containing anionic compounds (e.g., soaps or moisturizers with high pH), which neutralize its cationic properties. The CDC advises against combining chlorhexidine with incompatible products to maintain its efficacy. Option C, "Poor against gram positive bacteria," is incorrect. Chlorhexidine is highly effective against gram-positive bacteria (e.g., Staphylococcus aureus) and is often more potent against them than against gram-negative bacteria due to differences in cell wall structure, though it still has broad-spectrum activity.
The CBIC Practice Analysis (2022) supports the use of evidence-based antiseptics like chlorhexidine, and its persistent, broad-spectrum activity is well-documented in clinical studies (e.g., Larson, 1988, Journal of Hospital Infection). This makes Option D the most accurate statement regarding chlorhexidine soap’s microbial activity.
A patient has a draining sinus at the site of a left total hip arthroplasty. A culture from the sinus tract reveals four organisms. Which of the following specimens is optimal for identifying the eliologic agent?
Blood
Wound drainage
Joint aspirate
Sinus tract tissue
Theoptimal specimen for identifying the etiologic agentin a prosthetic joint infection (PJI) is ajoint aspirate(synovial fluid). This is because:
It provides direct access to the infected sitewithout contamination from external sources.
It allows for accurate microbiologic culture, Gram stain, and leukocyte count analysis.
Why the Other Options Are Incorrect?
A. Blood– Blood cultures may help detecthematogenous spreadbut are not the best sample for identifyinglocalizedprosthetic joint infections.
B. Wound drainage– Wound cultures oftencontain contaminantsfrom surrounding skin flora and do not accurately reflect joint space infection.
D. Sinus tract tissue– Cultures from sinus tracts often representcolonization rather than the primary infecting organism.
CBIC Infection Control Reference
APIC guidelines confirm thatjoint aspirate is the most reliable specimen for diagnosing prosthetic joint infections.
The infection preventionist (IP) collaborates with the Intravenous Therapy team to select the best antiseptic for use during the insertion of an intravascular device for adults. For a patient with no contraindications, what antiseptic should the IP suggest?
Chlorhexidine
Povidone-iodine
Alcohol
Antibiotic ointment
The selection of an appropriate antiseptic for the insertion of an intravascular device (e.g., peripheral or central venous catheters) is a critical infection prevention measure to reduce the risk of catheter-related bloodstream infections (CRBSIs). The Certification Board of Infection Control andEpidemiology (CBIC) emphasizes evidence-based practices in the "Prevention and Control of Infectious Diseases" domain, which includes adhering to guidelines for aseptic technique during invasive procedures. The Centers for Disease Control and Prevention (CDC) provides specific recommendations for skin antisepsis, as outlined in the "Guidelines for the Prevention of Intravascular Catheter-Related Infections" (2017).
Option A, chlorhexidine, is the preferred antiseptic for skin preparation prior to intravascular device insertion in adults with no contraindications. Chlorhexidine, particularly in a 2% chlorhexidine gluconate (CHG) with 70% isopropyl alcohol solution, is recommended by the CDC due to its broad-spectrum antimicrobial activity, residual effect (which continues to kill bacteria after application), and superior efficacy compared to other agents in reducing CRBSI rates. Studies cited in the CDC guidelines demonstrate that chlorhexidine-based preparations significantly lower infection rates compared to povidone-iodine or alcohol alone, making it the gold standard for this procedure when tolerated by the patient.
Option B, povidone-iodine, is an alternative antiseptic that can be used for skin preparation. It is effective against a wide range of microorganisms and is often used when chlorhexidine is contraindicated (e.g., in patients with chlorhexidine allergy). However, its efficacy is less persistent than chlorhexidine, and it requires longer drying time, which can be a limitation in busy clinical settings. The CDC considers povidone-iodine a second-line option unless chlorhexidine is unavailable or unsuitable. Option C, alcohol (e.g., 70% isopropyl or ethyl alcohol), has rapid bactericidal activity but lacks a residual effect, making it less effective for prolonged protection during catheter dwell time. It is often used as a component of chlorhexidine-alcohol combinations but is not recommended as a standalone antiseptic for intravascular device insertion. Option D, antibiotic ointment, is not appropriate for skin preparation during insertion. Antibiotic ointments (e.g., bacitracin or mupirocin) are sometimes applied to catheter sites post-insertion to prevent infection, but their use is discouraged by the CDC due to the risk of promoting antibiotic resistance and fungal infections, and they are not classified as antiseptics for initial skin antisepsis.
The CBIC Practice Analysis (2022) supports the adoption of CDC-recommended practices, and the 2017 CDC guidelines explicitly state that chlorhexidine-based preparations with alcohol should be used for skin antisepsis unless contraindicated. For a patient with no contraindications, the infection preventionist should suggest chlorhexidine to optimize patient safety and align with best practices.
The Infection Prevention and Control Committee is concerned about an outbreak of Serratia marcescens in the intensive care unit. If an environmental source is suspected, the BEST method to validate this suspicion is to
apply fluorescent gel.
use ATP system.
obtain surface cultures.
perform direct practice observation.
The correct answer is C, "obtain surface cultures," as this is the best method to validate the suspicion of an environmental source for an outbreak of Serratia marcescens in the intensive care unit (ICU). According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, Serratia marcescens is an opportunistic gram-negative bacterium commonly associated with healthcare-associated infections (HAIs), often linked to contaminated water, medical equipment, or environmental surfaces in ICUs. Obtaining surface cultures allows the infection preventionist (IP) to directly test environmental samples (e.g., from sinks, ventilators, or countertops) for the presence of Serratia marcescens, providing microbiological evidence to confirm or rule out an environmental source (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.2 - Analyze surveillance data). This method is considered the gold standard for outbreak investigations when an environmental reservoir issuspected, as it offers specific pathogen identification and supports targeted interventions.
Option A (apply fluorescent gel) is a technique used to assess cleaning efficacy by highlighting areas missed during disinfection, but it does not directly identify the presence of Serratia marcescens or confirm an environmental source. Option B (use ATP system) measures adenosine triphosphate (ATP) to evaluate surface cleanliness and organic residue, which can indicate poor cleaning practices, but it is not specific to detecting Serratia marcescens and lacks the diagnostic precision of cultures. Option D (perform direct practice observation) is valuable for assessing staff adherence to infection control protocols, but it addresses human factors rather than directly validating an environmental source, making it less relevant as the initial step in this context.
The focus on obtaining surface cultures aligns with CBIC’s emphasis on using evidence-based methods to investigate and control HAIs, enabling the IP to collaborate with the committee to pinpoint the source and implement corrective measures (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.3 - Identify risk factors for healthcare-associated infections). This approach is supported by CDC guidelines for outbreak investigations, which prioritize microbiological sampling to guide environmental control strategies (CDC Guidelines for Environmental Infection Control in Healthcare Facilities, 2019).
Which water type is suitable for drinking yet may still be a risk for disease transmission?
Purified water
Grey water
Potable water
Distilled water
To determine which water type is suitable for drinking yet may still pose a risk for disease transmission, we need to evaluate each option based on its definition, treatment process, and potential for contamination, aligning with infection control principles as outlined by the Certification Board of Infection Control and Epidemiology (CBIC).
A. Purified water: Purified water undergoes a rigorous treatment process (e.g., reverse osmosis, distillation, or deionization) to remove impurities, contaminants, and microorganisms. This results in water that is generally safe for drinking and has a very low risk of disease transmission when properly handled and stored. However, if the purification process is compromised or if contamination occurs post-purification (e.g., due to improper storage or distribution), there could be a theoretical risk. Nonetheless, purified water is not typically considered a primary source of disease transmission under standard conditions.
B. Grey water: Grey water refers to wastewater generated from domestic activities such as washing dishes, laundry, or bathing, which may contain soap, food particles, and small amounts of organic matter. It is not suitable for drinking due to its potential contaminationwith pathogens (e.g., bacteria, viruses) and chemicals. Grey water is explicitly excluded from potable water standards and poses a significant risk for disease transmission, making it an unsuitable choice for this question.
C. Potable water: Potable water is water that meets regulatory standards for human consumption, as defined by organizations like the World Health Organization (WHO) or the U.S. Environmental Protection Agency (EPA). It is treated to remove harmful pathogens and contaminants, making it safe for drinking under normal circumstances. However, despite treatment, potable water can still pose a risk for disease transmission if the distribution system is contaminated (e.g., through biofilms, cross-connections, or inadequate maintenance of pipes). Outbreaks of waterborne diseases like Legionnaires' disease or gastrointestinal infections have been linked to potable water systems, especially in healthcare settings. This makes potable water the best answer, as it is suitable for drinking yet can still carry a risk under certain conditions.
D. Distilled water: Distilled water is produced by boiling water and condensing the steam, which removes most impurities, minerals, and microorganisms. It is highly pure and safe for drinking, often used in medical and laboratory settings. Similar to purified water, the risk of disease transmission is extremely low unless contamination occurs after distillation due to improper handling or storage. Like purified water, it is not typically associated with disease transmission risks in standard use.
The key to this question lies in identifying a water type that is both suitable for drinking and has a documented potential for disease transmission. Potable water fits this criterion because, while it is intended for consumption and meets safety standards, it can still be a vector for disease if the water supply or distribution system is compromised. This is particularly relevant in infection control, where maintaining water safety in healthcare facilities is a critical concern addressed by CBIC guidelines.
When implementing a multimodal strategy (or bundle) for improving hand hygiene, the infection preventionist should focus on Calculator
signage for hand hygiene reminders.
cost effectiveness of hand hygiene products.
availability of gloves in the patient care area
institutional assessment of significant barriers.
When implementing amultimodal strategy (or bundle) for hand hygiene, the infection preventionist shouldfirst assess barriers to compliancebefore implementing solutions.
Step-by-Step Justification:
Understanding Barriers First:
Identifying barriers(e.g., lack of access to sinks, high workload, or poor compliance culture)is critical for effective intervention.
APIC Guidelines on Hand Hygiene Improvement:
Strategiesmust be tailoredbased on the institution's specific challenges.
Why Other Options Are Incorrect:
A. Signage for hand hygiene reminders:
Signagealoneis insufficient without addressingsystemic barriers.
B. Cost-effectiveness of hand hygiene products:
While important,cost analysis comes after identifying compliance barriers.
C. Availability of gloves in the patient care area:
Gloves do not replace hand hygiene and maylead to lower compliance.
CBIC Infection Control References:
APIC/JCR Workbook, "Hand Hygiene Compliance and Institutional Barriers".
APIC Text, "Hand Hygiene Improvement Strategies".
There are four cases of ventilator-associated pneumonia in a surgical intensive care unit with a total of 200 ventilator days and a census of 12 patients. Which of the following BEST expresses how this should be reported?
Ventilator-associated pneumonia rate of 2%
20 ventilator-associated pneumonia cases/1000 ventilator days
Postoperative pneumonia rate of 6% in SICU patients
More information is needed regarding ventilator days per patient
The standard way to reportventilator-associated pneumonia (VAP) ratesis:
 A white paper with black text
AI-generated content may be incorrect.
A white paper with black text
AI-generated content may be incorrect.
Why the Other Options Are Incorrect?
A. Ventilator-associated pneumonia rate of 2%– This does not use thecorrect denominator (ventilator days).
C. Postoperative pneumonia rate of 6% in SICU patients–Not relevant, as the data focuses onVAP, not postoperative pneumonia.
D. More information is needed regarding ventilator days per patient–The total ventilator days are already provided, so no additional data is required.
CBIC Infection Control Reference
APIC and NHSN recommend reporting VAP rates as cases per 1,000 ventilator days.
An 84-year-old male with a gangrenous foot is admitted to the hospital from an extended-care facility (ECF). The ECF is notified that the wound grew Enterococcus faecium with the followingantibiotic sensitivity results:
ampicillin – R
vancomycin – R
penicillin – R
linezolid – S
This is the fourth Enterococcus species cultured from residents within the same ECF wing in the past month. The other cultures were from two urine specimens and a draining wound. The Infection Preventionist (IP) should immediately:
Notify the medical director of the outbreak.
Compare the four culture reports and sensitivity patterns.
Conduct surveillance cultures for this organism in all residents.
Notify the nursing administrator to close the wing to new admissions.
The scenario describes a potential outbreak of multidrug-resistant Enterococcus faecium in an extended-care facility (ECF) wing, indicated by four positive cultures (including the current case and three prior cases from urine and a draining wound) within a month. The organism exhibits resistance to ampicillin, vancomycin, and penicillin, but sensitivity to linezolid, suggesting a possible vancomycin-resistant Enterococcus (VRE) strain, which is a significant concern in healthcare settings. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes the importance of rapid outbreak detection and response in the "Surveillance and Epidemiologic Investigation" domain, aligning with Centers for Disease Control and Prevention (CDC) guidelines for managing multidrug-resistant organisms (MDROs).
Option A, "Notify the medical director of the outbreak," is the most immediate and critical action. Identifying an outbreak—defined by the CDC as two or more cases of a similar illness linked by time and place—requires prompt notification to the facility’s leadership (e.g., medical director) to initiate a coordinated response. The presence of four Enterococcus cases, including a multidrug-resistant strain, within a single ECF wing over a month suggests a potential cluster, necessitating urgent action to assess the scope, implement control measures, and allocate resources. The CDC’s "Management of Multidrug-Resistant Organisms in Healthcare Settings" (2006) recommends immediate reporting to facility leadership as the first step to activate an outbreak investigation team, making this the priority.
Option B, "Compare the four culture reports and sensitivity patterns," is an important subsequent step in outbreak investigation. Analyzing the antibiotic susceptibility profiles and culture sources can confirm whether the cases are epidemiologically linked (e.g., clonal spread of VRE) and guide treatment and control strategies. However, this is a detailed analysis that follows initial notification and should not delay alerting the medical director. Option C, "Conduct surveillance cultures for this organism in all residents," is a proactive measure to determine the prevalence of Enterococcus faecium, especially VRE, within the wing. The CDC recommends targeted surveillance during outbreaks, but this requires prior authorization and planning by the outbreak team, making it a secondary action after notification. Option D, "Notify the nursing administrator to close the wing to new admissions," may be a control measure to prevent further spread, as suggested by the CDC for MDRO outbreaks. However, closing a unit is a significant decision that should be guided by the medical director and infection control team after assessing the situation, not an immediate independent action by the IP.
The CBIC Practice Analysis (2022) and CDC guidelines prioritize rapid communication with leadership to initiate a structured outbreak response, including resource allocation and policy adjustments. Given the multidrug-resistant nature and cluster pattern, notifying the medical director (Option A) is the most immediate and appropriate action to ensure a comprehensive response.
An infection preventionist in the role of educator is teaching risk reduction activities to patients and families. For which of the following groups is the pneumococcal vaccine MOST appropriate?
Asplenic patients
International travelers
Immunocompromised newborns
Patients in behavioral health settings
The pneumococcal vaccine is designed to protect against infections caused by Streptococcus pneumoniae, a bacterium responsible for diseases such as pneumonia, meningitis, and bacteremia. The appropriateness of this vaccine depends on the population's risk profile, particularly their susceptibility to invasive pneumococcal disease (IPD). The Certification Board of Infection Control and Epidemiology (CBIC) highlights the role of infection preventionists as educators in promoting vaccination as a key risk reduction strategy, aligning with the "Education and Training" domain (CBIC Practice Analysis, 2022). The Centers for Disease Control and Prevention (CDC) provides specific guidelines on pneumococcal vaccination, recommending it for individuals at higher risk due to underlying medical conditions or immunologic status.
Option A, asplenic patients, refers to individuals who have had their spleen removed (e.g., due to trauma or disease) or have a nonfunctional spleen (e.g., in sickle cell disease). The spleen plays a critical role in clearing encapsulated bacteria like Streptococcus pneumoniae from the bloodstream. Without a functioning spleen, these patients are at significantly increased risk of overwhelming post-splenectomy infection (OPSI), with pneumococcal disease being a leading cause. The CDC and Advisory Committee on Immunization Practices (ACIP) strongly recommend pneumococcal vaccination, including both PCV15/PCV20 and PPSV23, for asplenic patients, making this group the most appropriate for the vaccine in this context. The infection preventionist should prioritize educating these patients and their families about the vaccine's importance and timing.
Option B, international travelers, may benefit from various vaccines depending on their destination (e.g., yellow fever or typhoid), but pneumococcal vaccination is not routinely recommended unless they have specific risk factors (e.g., asplenia or chronic illness) or are traveling to areas with high pneumococcal disease prevalence. This group is not inherently a priority for pneumococcal vaccination. Option C, immunocompromised newborns, includes infants with congenital immunodeficiencies or other conditions, who may indeed require pneumococcal vaccination as part of their routine immunization schedule (e.g., PCV15 or PCV20 starting at 2 months). However, newborns are generally covered under universal childhood vaccination programs, and the question’s focus on "MOST appropriate" suggests a group with a more specific, elevated risk, which asplenic patients fulfill. Option D, patients in behavioral health settings, may have varied health statuses, but this group is not specifically targeted for pneumococcal vaccination unless they have additional risk factors (e.g., chronic diseases), making it less appropriate than asplenic patients.
The CBIC emphasizes tailoring education to high-risk populations, and the CDC’s Adult and Pediatric Immunization Schedules (2023) identify asplenic individuals as a top priority for pneumococcal vaccination due to their extreme vulnerability. Thus, the infection preventionist should focus on asplenic patients as the group for whom the pneumococcal vaccine is most appropriate.
The infection preventionist and Occupational Health discuss the 65% influenza vaccination rate for healthcare personnel. Which is MOST effective method to increase compliance?
Pre-schedule healthcare personnel for vaccine administration
Require annual vaccine as a condition of employment
Educate staff about risks of not receiving vaccine
Offer the vaccine year round to increase compliance
Requiring influenza vaccination as acondition of employmenthas consistently been shown to be the most effective method to increase compliance among healthcare personnel.
TheAPIC/JCR Workbookrecommends this as a gold standard:
"Some organizations have adopted policies requiring annual vaccination as a condition of employment unless medically contraindicated".
CDC and APIC also support this method for maximizing coverage and protecting vulnerable populations.
Which of the following intravenous solutions will MOST likely promote the growth of microorganisms?
50% hypertonic glucose
5% dextrose
Synthetic amino acids
10% lipid emulsions
10% lipid emulsionsare themost likely to promote microbial growthbecause they provide an ideal environment forbacterial and fungal proliferation, especiallyStaphylococcus aureus, Pseudomonas aeruginosa, and Candida species. Lipids supportrapid bacterial multiplicationdue to theirhigh nutrient content.
Why the Other Options Are Incorrect?
A. 50% hypertonic glucose–High glucose concentrations inhibit bacterial growthdue toosmotic pressure effects.
B. 5% dextrose– While it can support some bacterial growth, it isless favorablethan lipid emulsions.
C. Synthetic amino acids– These solutionsdo not support microbial growth as well as lipid emulsions.
CBIC Infection Control Reference
APIC guidelines confirm that lipid-based solutions support rapid microbial growthand should be handled with strict aseptic technique.
Infection Prevention and Control identified a cluster of Aspergillus fumigatus infections in the transplant unit. The infection preventionist (IP) meets with the unit director and Environmental Services director to begin investigation. What information does the IP need from the Environmental Services director?
Date of last terminal clean of the infected patient rooms
Hospital grade disinfectant used on the transplant unit
Use of dust mitigating strategies during floor care
Date of the last cleaning of the fish tank in the waiting room
The correct answer is A, "Date of last terminal clean of the infected patient rooms," as this is the most critical information the infection preventionist (IP) needs from the Environmental Services director to begin the investigation of a cluster of Aspergillus fumigatus infections in the transplant unit. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, Aspergillus fumigatus is an environmental fungus that thrives in areas with poor ventilation, construction dust, or inadequate cleaning, posing a significant risk to immunocompromised patients, such as those in transplant units. A terminal clean—thorough disinfection and cleaning of a patient room after discharge or transfer—is a key infection control measure to eliminate fungal spores and other pathogens (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.4 - Implement environmental cleaning and disinfection protocols). Determining the date of the last terminal clean helps the IP assess whether lapses in cleaning schedules or procedures could have contributed to the cluster, guiding further environmental sampling or process improvements.
Option B (hospital grade disinfectant used on the transplant unit) is relevant to the investigation but is secondary; the IP would need to know the cleaning schedule first to contextualize the disinfectant’s effectiveness. Option C (use of dust mitigating strategies during floor care) is important, as Aspergillus spores can be aerosolized during floor maintenance, but this is a specific procedural detail that follows the initial focus on cleaning history. Option D (date of the last cleaning of the fish tank in the waiting room) is unlikely to be a priority unless evidence suggests a direct link to the transplant unit, which is not indicated here; Aspergillus is more commonly associated with air quality and room cleaning rather than fish tanks.
The focus on the date of the last terminal clean aligns with CBIC’s emphasis on investigating environmental factors in healthcare-associated infection (HAI) clusters, enabling the IP to collaborate with Environmental Services to pinpoint potential sources and implement corrective actions (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.2 - Analyze surveillance data). This step is foundational to controlling the outbreak and protecting vulnerable patients.
Which of the following options describes a correct use of personal protective equipment?
Personal eyeglasses should be worn during suctioning.
Surgical masks should be worn during lumbar puncture procedures.
Gloves should be worn when handling or touching a cardiac monitor that has been disinfected.
Eye protection should be worn when providing patient care it at risk of spreading respiratory disease after unprotected exposure.
According toCDC and APIC guidelines, asurgical mask is requiredwhen performinglumbar puncturestoprevent bacterial contamination (e.g., meningitis caused by droplet transmission of oral flora).
Why the Other Options Are Incorrect?
A. Personal eyeglasses should be worn during suctioning–Incorrectbecauseeyeglasses do not provide adequate eye protection. Goggles or face shields should be used.
C. Gloves should be worn when handling or touching a cardiac monitor that has been disinfected–Not necessaryunless recontamination is suspected.
D. Eye protection should be worn when providing patient care after unprotected exposure– Eye protection should be usedbefore exposure, not just after.
CBIC Infection Control Reference
APIC states that surgical masks must be worn for procedures such as lumbar puncture to reduce infection risk.
The infection preventionist (IP) is working with the Product Evaluation Committee to select a sporicidal disinfectant for Clostridioides difficile. An effective disinfectant for the IP to recommend is
quaternary ammonium compound.
phenolic.
isopropyl alcohol.
sodium hypochlorite.
The correct answer is D, "sodium hypochlorite," as it is an effective sporicidal disinfectant for Clostridioides difficile that the infection preventionist (IP) should recommend. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, Clostridioides difficile (C. difficile) is a spore-forming bacterium responsible for significant healthcare-associated infections (HAIs), and its spores are highly resistant to many common disinfectants. Sodium hypochlorite (bleach) is recognized by the Centers for Disease Control and Prevention (CDC) and the Environmental Protection Agency (EPA) as a sporicidal agent capable of inactivating C. difficile spores when used at appropriate concentrations (e.g., 1:10 dilution of household bleach) and with the recommended contact time (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.4 - Implement environmental cleaning and disinfection protocols). This makes it a preferred choice for environmental disinfection in outbreak settings or areas with known C. difficile contamination.
Option A (quaternary ammonium compound) is effective against many bacteria and viruses but lacks sufficient sporicidal activity against C. difficile spores, rendering it inadequate for this purpose. Option B (phenolic) has broad-spectrum antimicrobial properties but is not reliably sporicidal and is less effective against C. difficile spores compared to sodium hypochlorite. Option C (isopropyl alcohol) is useful for disinfecting surfaces and killing some pathogens, but it is not sporicidal and evaporates quickly, making it ineffective against C. difficile spores.
The IP’s recommendation of sodium hypochlorite aligns with CBIC’s emphasis on selecting disinfectants based on their efficacy against specific pathogens and adherence to evidence-based guidelines (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.5 - Evaluate the environment for infection risks). Proper use, including correct dilution and contact time, is critical to ensure effectiveness, and the IP should collaborate with the Product Evaluation Committee to ensure implementation aligns with safety and regulatory standards (CDC Guidelines for Environmental Infection Control in Healthcare Facilities, 2019).
Which of the following strategies is MOST effective in reducing surgical site infections (SSI) in orthopedic procedures?
Perioperative normothermia maintenance.
Routine intraoperative wound irrigation with povidone-iodine.
Administration of prophylactic antibiotics postoperatively for 48 hours.
Use of sterile adhesive wound dressings for 10 days postoperatively.
Perioperative normothermia maintenance reduces SSI rates by improving immune function and tissue perfusion.
Routine wound irrigation (B) has no strong evidence supporting SSI prevention.
Prolonged antibiotic use (C) increases antibiotic resistance without added benefit.
Extended use of wound dressings (D) does not reduce SSI rates.
CBIC Infection Control References:
APIC Text, "SSI Prevention in Surgery," Chapter 12.
An adult with an incomplete vaccination history presents with an uncontrollable, rapid and violent cough, fever, and runny nose. Healthcare personnel should suspect
Pertussis.
Rhinovirus.
Bronchitis.
Adenovirus.
The correct answer is A, "Pertussis," as healthcare personnel should suspect this condition based on the presented symptoms and the patient’s incomplete vaccination history. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, pertussis, caused by the bacterium Bordetella pertussis, is characterized by an initial phase of mild respiratory symptoms (e.g., runny nose, low-grade fever) followed by a distinctive uncontrollable, rapid, and violent cough, often described as a "whooping" cough. This presentation is particularly concerning in adults with incomplete vaccination histories, as the pertussis vaccine’s immunity (e.g., DTaP or Tdap) wanes over time, increasing susceptibility (CBIC Practice Analysis, 2022, Domain I: Identification of Infectious Disease Processes, Competency 1.1 - Identify infectious disease processes). Pertussis is highly contagious and poses a significant risk in healthcare settings, necessitating prompt suspicion and isolation to prevent transmission.
Option B (rhinovirus) typically causes the common cold with symptoms like runny nose, sore throat, and mild cough, but it lacks the violent, paroxysmal cough characteristic of pertussis. Option C (bronchitis) may involve cough and fever, often due to viral or bacterial infection, but it is not typically associated with the rapid and violent cough pattern or linked to vaccination status in the same way as pertussis. Option D (adenovirus) can cause respiratory symptoms, including cough and fever, but it is more commonly associated with conjunctivitis or pharyngitis and does not feature the hallmark violent cough of pertussis.
The suspicion of pertussis aligns with CBIC’s emphasis on recognizing infectious disease patterns to initiate timely infection control measures, such as droplet precautions and prophylaxis for exposed individuals (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.2 - Implement measures to prevent transmission of infectious agents). Early identification is critical, especially in healthcare settings, to protect vulnerable patients and staff, and the incomplete vaccination history supports this differential diagnosis given pertussis’s vaccine-preventable nature (CDC Pink Book: Pertussis, 2021).
Which of the following is the correct collection technique to obtain a laboratory specimen for suspected pertussis?
Cough plate
Nares culture
Sputum culture
Nasopharyngeal culture
Thegold standard specimenfor diagnosingpertussis (Bordetella pertussis infection)is anasopharyngeal culturebecause:
B. pertussis colonizes the nasopharynx, making it the best site for detection.
Aproperly collected nasopharyngeal swab or aspirateincreases diagnostic sensitivity.
This method is recommended forculture, PCR, or direct fluorescent antibody testing.
Why the Other Options Are Incorrect?
A. Cough plate– Not commonly used due tolow sensitivity.
B. Nares culture– Thenares are not a primary sitefor pertussis colonization.
C. Sputum culture–B. pertussis does not commonly infect the lower respiratory tract.
CBIC Infection Control Reference
APIC confirms thatnasopharyngeal culture is the preferred method for diagnosing pertussis.
An infection preventionist (IP) is tasked with developing an infection prevention training program for family members. What step should the IP take FIRST?
Assess the needs of the family members at the facility.
Create clearly defined goals and objectives for the training.
Ensure that all content in the training is relevant and practical.
Develop a plan to create an appropriate training environment.
The correct answer is A, "Assess the needs of the family members at the facility," as this is the first step the infection preventionist (IP) should take when developing an infection prevention training program for family members. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, effective education programs begin with a needs assessment to identify the specific knowledge gaps, cultural factors, and practical challenges of the target audience—in this case, family members. This initial step ensures that the training is tailored to their level of understanding, language preferences, and the infection risks they may encounter (e.g., hand hygiene, isolation protocols), aligning with adult learning principles (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.1 - Develop and implement educational programs). Without this assessment, subsequent steps risk being misaligned with the audience’s needs, reducing the program’s effectiveness.
Option B (create clearly defined goals and objectives for the training) is a critical step but follows the needs assessment, as goals should be based on identified needs to ensure relevance. Option C (ensure that all content in the training is relevant and practical) depends on understanding the audience’s needs first, making it a later step in the development process. Option D (develop a plan to create an appropriate training environment) is important for implementation but requires prior knowledge of the audience and content to design effectively.
The focus on assessing needs aligns with CBIC’s emphasis on evidence-based education design,enabling the IP to address specific infection prevention priorities for family members and improve outcomes in the facility (CBIC Practice Analysis, 2022, Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs). This approach is supported by CDC guidelines, which recommend audience assessment as a foundational step in health education programs.
Immediate use steam sterilization is NOT recommended for implantable items requiring immediate use because
the high temperature may damage the items.
chemical indicators may not be accurate at high temperatures.
results of biologic indicators are unavailable prior to use of the item.
the length of time is inadequate for the steam to penetrate the pack.
The correct answer is C, "results of biologic indicators are unavailable prior to use of the item," as this is the primary reason immediate use steam sterilization (IUSS) is not recommended for implantable items requiring immediate use. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, IUSS is a process used for sterilizing items needed urgently when no other sterile options are available, typically involving a shortened cycle (e.g., flash sterilization). However, for implantable items—such as orthopedic hardware or prosthetic devices—ensuring absolute sterility is critical due to the risk of deep infection. Biologic indicators (BIs), which contain highly resistant spores to verify sterilization efficacy, require incubation (typically 24-48 hours) to confirm the kill, but IUSS does not allow time for BI results to be available before the item is used (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.3 - Ensure safe reprocessing of medical equipment). This lack of immediate verification poses a significant infection risk, making IUSS inappropriate for implants, as per AAMI ST79 standards.
Option A (the high temperature may damage the items) is a consideration for some heat-sensitive materials, but modern IUSS cycles are designed to minimize damage, and this is not the primary reason for the restriction on implants. Option B (chemical indicators may not be accurate at high temperatures) is incorrect, as chemical indicators (e.g., color-changing strips) are reliable at high temperatures and serve as an immediate check, though they are not a substitute for BIs. Option D (the length of time is inadequate for the steam to penetrate the pack) is not the main issue, as IUSS cycles are optimized for penetration, though the shortened time may be a secondary concern; the unavailability of BI results remains the decisive factor.
The focus on biologic indicator results aligns with CBIC’s emphasis on ensuring the safety and sterility of reprocessed medical devices, particularly for high-risk implantable items (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.5 - Evaluate the environment for infection risks). This recommendation is supported by AAMI and CDC guidelines, which prioritize BI confirmation for implants to prevent healthcare-associated infections (AAMI ST79:2017, CDC Sterilization Guidelines, 2019).
A Quality Improvement Committee is trying to decrease catheter-associated urinary tract infections (CAUTIs) in the hospital. Which of the following would be an outcome measure that would help to show a reduction in CAUTIs?
Rate of patients receiving daily indwelling urinary catheter care
Percentage of patients with indwelling urinary catheters
Rate of CAUTI per 1000 indwelling urinary catheter days
Percentage of staff trained to insert indwelling urinary catheters
Anoutcome measuretracks the end result of healthcare processes. TheCAUTI rate per 1,000 catheter daysdirectly measures the frequency of infections, making it an ideal outcome metric.
From theAPIC Text:
“An incidence rate (i.e., the number of new cases during a time period, such as the rate of patients with urinary catheters who get a CAUTI) is a frequently used outcome performance measure.”
Other choices like care compliance or training areprocess measures, not outcomes.
Which of the following individuals should be excluded from receiving live attenuated influenza virus?
Pregnant persons
Healthy persons aged 2 to 49
Persons with allergies to chicken feathers
Persons simultaneously receiving an inactivated vaccine
The correct answer is A, "Pregnant persons," as they should be excluded from receiving the live attenuated influenza virus (LAIV) vaccine. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, which align with recommendations from the Centers for Disease Control and Prevention (CDC) and the Advisory Committee on Immunization Practices (ACIP), the LAIV, commonly known as the nasal spray flu vaccine, contains a live attenuated form of the influenza virus. This vaccine is contraindicated in pregnant individuals due to the theoretical risk of the attenuated virus replicating and potentially harming the fetus, despite limited evidence of adverse outcomes (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.2 - Implement measures to prevent transmission of infectious agents). Pregnant persons are instead recommended to receive the inactivated influenza vaccine (IIV), which is considered safe during pregnancy.
Option B (healthy persons aged 2 to 49) is incorrect because this group is generally eligible to receive LAIV, provided they have no other contraindications, as the vaccine is approved for healthy, non-pregnant individuals in this age range (CDC Immunization Schedules, 2024). Option C (persons with allergies to chicken feathers) is not a contraindication for LAIV; the vaccine isproduced in eggs, and while egg allergy was historically a concern, current guidelines indicate that LAIV can be administered to persons with egg allergies if they can tolerate egg in their diet, with precautions managed by healthcare providers. Option D (persons simultaneously receiving an inactivated vaccine) is also incorrect, as LAIV can be co-administered with inactivated vaccines without issue, according to ACIP recommendations, as there is no significant interference between the two vaccine types.
The exclusion of pregnant persons reflects CBIC’s emphasis on tailoring infection prevention strategies, including vaccination programs, to protect vulnerable populations while minimizing risks (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.1 - Collaborate with organizational leaders). This decision is based on precautionary principles outlined in CDC and ACIP guidelines to ensure maternal and fetal safety (CDC Prevention and Control of Seasonal Influenza with Vaccines, 2023).
Following recent renovations on an oncology unit, three patients were identified with Aspergillus infections. The infections were thought to be facility-acquired. Appropriate environmental microbiological monitoring would be to culture the:
Air
Ice
Carpet
Aerators
The scenario describes an outbreak of Aspergillus infections among three patients on an oncology unit following recent renovations, with the infections suspected to be facility-acquired. Aspergillus is a mold commonly associated with environmental sources, particularly airborne spores, and its presence in immunocompromised patients (e.g., oncology patients) poses a significant risk. The infection preventionist must identify the appropriate environmental microbiological monitoring strategy, guided by the Certification Board of Infection Control and Epidemiology (CBIC) and CDC recommendations. Let’s evaluate each option:
A. Air: Aspergillus species are ubiquitous molds that thrive in soil, decaying vegetation, and construction dust, and they are primarily transmitted via airborne spores. Renovations can disturb these spores, leading to aerosolization and inhalation by vulnerable patients. Culturing the air using methods such as settle plates, air samplers, or high-efficiency particulate air (HEPA) filtration monitoring is a standard practice to detect Aspergillusduring construction or post-renovation in healthcare settings, especially oncology units where patients are at high risk for invasive aspergillosis. This aligns with CBIC’s emphasis on environmental monitoring for airborne pathogens, making it the most appropriate choice.
B. Ice: Ice can be a source of contamination with bacteria (e.g., Pseudomonas, Legionella) or other pathogens if improperly handled or stored, but it is not a typical reservoir for Aspergillus, which is a mold requiring organic material and moisture for growth. While ice safety is important in infection control, culturing ice is irrelevant to an Aspergillus outbreak linked to renovations and is not a priority in this context.
C. Carpet: Carpets can harbor dust, mold, and other microorganisms, especially in high-traffic or poorly maintained areas. Aspergillus spores could theoretically settle in carpet during renovations, but carpets are not a primary source of airborne transmission unless disturbed (e.g., vacuuming). Culturing carpet might be a secondary step if air sampling indicates widespread contamination, but it is less direct and less commonly recommended as the initial monitoring site compared to air sampling.
D. Aerators: Aerators (e.g., faucet aerators) can harbor waterborne pathogens like Pseudomonas or Legionella due to biofilm formation, but Aspergillus is not typically associated with water systems unless there is significant organic contamination or aerosolization from water sources (e.g., cooling towers). Culturing aerators is relevant for waterborne outbreaks, not for an Aspergillus outbreak linked to renovations, making this option inappropriate.
The best answer is A, culturing the air, as Aspergillus is an airborne pathogen, and renovations are a known risk factor for spore dispersal in healthcare settings. This monitoring strategy allows the infection preventionist to confirm the source, assess the extent of contamination, and implement control measures (e.g., enhanced filtration, construction barriers) to protect patients. This is consistent with CBIC and CDC guidelines for managing fungal outbreaks in high-risk units.
Which of the following patients with human immunodeficiency virus infection requires Airborne precautions?
24-year-old male newly diagnosed with a CD4 count of 70
28-year-old female with Mycobacterium avium in sputum
36-year-old male with cryptococcal meningitis
46-year-old female with a cavitary lesion in upper lobe
HIV patients require Airborne Precautions if they have tuberculosis (TB).Acavitary lesion in the upper lobeishighly suggestive of active pulmonary TB, which requiresAirborne Precautionsdue toaerosolized transmission.
Why the Other Options Are Incorrect?
A. 24-year-old male newly diagnosed with a CD4 count of 70–Low CD4 count alone does not warrant Airborne Precautionsunless there isactive TB or another airborne pathogen.
B. 28-year-old female with Mycobacterium avium in sputum–Mycobacterium avium complex (MAC) is not airborne, and standard precautions are sufficient.
C. 36-year-old male with cryptococcal meningitis–Cryptococcus neoformans is not transmitted via the airborne route, so Airborne Precautions are unnecessary.
CBIC Infection Control Reference
Patients withHIV and suspected TB require Airborne Precautionsuntil TB is ruled out.
An infection preventionist is reviewing employee health immunization policies. What is the recommendation for tetanus toxoid, reduced diphtheria toxoid, and acellular pertussis (Tdap) for a 55-year-old nurse who received all childhood vaccinations?
One dose of Tdap vaccine
Two doses of Tdap vaccine at least 14 days apart
Two doses of Tdap vaccine at least 28 days apart
No additional vaccination is recommended
The correct answer is A, "One dose of Tdap vaccine," as this is the recommended immunization for a 55-year-old nurse who received all childhood vaccinations. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, which align with recommendations from the Centers for Disease Control and Prevention (CDC) and the Advisory Committee on Immunization Practices (ACIP), adults who have completed a primary series of childhood vaccinations (typically 5 doses of DTaP or DTP) should receive a single booster dose of Tdap if they have not previously received it. This is especially critical for healthcare personnel, such as a 55-year-old nurse, due to their increased risk of exposure to pertussis and the need to protectvulnerable patients (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.2 - Implement measures to prevent transmission of infectious agents). The Tdap vaccine, which protects against tetanus, diphtheria, and pertussis, is recommended once between ages 11-64, with a preference for administration in early adulthood (e.g., 19-26 years) or as soon as feasible for older adults, including this 55-year-old nurse, to ensure immunity against pertussis, which wanes over time. For individuals aged 65 and older, Tdap is still recommended if not previously received, though Tdap is preferred over Td (tetanus and diphtheria only) for healthcare workers to address pertussis risk.
Option B (two doses of Tdap vaccine at least 14 days apart) and Option C (two doses of Tdap vaccine at least 28 days apart) are not standard recommendations for adults with a complete childhood vaccination history. Multiple doses are typically reserved for individuals with incomplete primary series or specific high-risk conditions, not for this scenario. Option D (no additional vaccination is recommended) is incorrect because, even with a complete childhood series, a Tdap booster is advised for healthcare workers to maintain protection, especially given the nurse’s occupational exposure risks (CDC Immunization Schedules, 2024). After receiving the Tdap booster, a Td booster every 10 years is recommended to maintain tetanus and diphtheria immunity, but the initial Tdap dose is the priority for this nurse.
The recommendation for one Tdap dose aligns with CBIC’s emphasis on evidence-based immunization policies to prevent transmission of vaccine-preventable diseases in healthcare settings (CBIC Practice Analysis, 2022, Domain III: Infection Prevention and Control, Competency 3.1 - Collaborate with organizational leaders). This ensures the nurse is protected and contributes to herd immunity, reducing the risk of pertussis outbreaks in the healthcare environment.
A healthcare facility has installed a decorative water fountain in their lobby for the enjoyment of patients and visitors. What is an important issue for the infection preventionist to consider?
Children getting Salmonella enteritidis
Cryptosporidium growth in the fountain
Aerosolization of Legionella pneumophila
Growth of Acinetobacter baumannii
The installation of a decorative water fountain in a healthcare facility lobby introduces a potential environmental hazard that an infection preventionist must evaluate, guided by the Certification Board of Infection Control and Epidemiology (CBIC) principles and infection control best practices. Water features can serve as reservoirs for microbial growth and dissemination, particularly in settings with vulnerable populations such as patients. The key is to identify the most significant infection risk associated with such a water source. Let’s analyze each option:
A. Children getting Salmonella enteritidis: Salmonella enteritidis is a foodborne pathogen typically associated with contaminated food or water sources like poultry, eggs, or untreated drinking water. While children playing near a fountain might theoretically ingest water, Salmonella is not a primary concern for decorative fountains unless they are specifically contaminated with fecal matter, which is uncommon in a controlled healthcare environment. This risk is less relevant compared to other waterborne pathogens.
B. Cryptosporidium growth in the fountain: Cryptosporidium is a parasitic protozoan that causes gastrointestinal illness, often transmitted through contaminated drinking water or recreational water (e.g., swimming pools). While decorative fountains could theoretically harbor Cryptosporidium if contaminated, this organism requires specific conditions (e.g., fecal contamination) and is more associated with untreated or poorly maintained water systems. In a healthcare setting with regular maintenance, this is a lower priority risk compared to bacterial pathogens spread via aerosols.
C. Aerosolization of Legionella pneumophila: Legionella pneumophila is a gram-negative bacterium that thrives in warm, stagnant water environments, such as cooling towers, hot water systems, and decorative fountains. It causes Legionnaires’ disease, a severe form of pneumonia, and Pontiac fever, both transmitted through inhalation of contaminated aerosols. In healthcare facilities, where immunocompromised patients are present, aerosolization from a water fountain poses a significant risk, especially if the fountain is not regularly cleaned, disinfected, or monitored. The CBIC and CDC highlight Legionella as a critical concern in water management programs, making this the most important issue for an infection preventionist to consider.
D. Growth of Acinetobacter baumannii: Acinetobacter baumannii is an opportunistic pathogen commonly associated with healthcare-associated infections (e.g., ventilator-associated pneumonia, wound infections), often found on medical equipment or skin. While it can survive in moist environments, its growth in a decorative fountain is less likely compared to Legionella, which is specifically adapted to water systems. The risk ofAcinetobacter transmission via a fountain is minimal unless it becomes a direct contamination source, which is not a primary concern for this scenario.
The most important issue is C, aerosolization of Legionella pneumophila, due to its potential to cause severe respiratory infections, its association with water features, and the heightened vulnerability of healthcare facility populations. The infection preventionist should ensure the fountain is included in the facility’s water management plan, with regular testing, maintenance, and disinfection to prevent Legionella growth and aerosol spread, as recommended by CBIC and CDC guidelines.
An infection preventionist is utilizing the Shewhart/Deming cycle in an infection control program performance improvement project. In which of the following steps are the results of the interventions compared with the original goal?
Do
Act
Plan
Study
The correct answer is D, "Study," as this is the step in the Shewhart/Deming cycle (commonly known as the Plan-Do-Study-Act [PDSA] cycle) where the results of the interventions are compared with the original goal. According to the Certification Board of Infection Control and Epidemiology (CBIC) guidelines, the PDSA cycle is a systematic approach to quality improvement, widely used in infection control programs to test and refine interventions. The cycle consists of four stages: Plan (designing the intervention and setting goals), Do (implementing the intervention on a small scale), Study (analyzing the data and comparing outcomes against the original goal), and Act (standardizing successful changes or adjusting based on findings) (CBIC Practice Analysis, 2022,Domain IV: Education and Research, Competency 4.2 - Evaluate the effectiveness of educational programs). The Study phase is critical for assessing whether the intervention achieved the intended reduction in infection rates or other performance metrics, providing evidence to guide the next steps.
Option A (Do) involves the execution of the planned intervention, focusing on implementation rather than evaluation, so it does not include comparing results. Option B (Act) is the final step where successful interventions are implemented on a broader scale or adjustments are made, but it follows the comparison made in the Study phase. Option C (Plan) is the initial stage of setting objectives and designing the intervention, which occurs before any results are available for comparison.
The emphasis on the Study phase aligns with CBIC’s focus on using data to evaluate the effectiveness of infection prevention strategies, ensuring that performance improvement projects are evidence-based and goal-oriented (CBIC Practice Analysis, 2022, Domain II: Surveillance and Epidemiologic Investigation, Competency 2.4 - Evaluate the effectiveness of infection prevention and control interventions). This step enables the infection preventionist to determine if the original goal—such as reducing healthcare-associated infections—was met, facilitating continuous improvement.
An infection preventionist has been informed that a patient admitted 2 days ago has been diagnosed with chickenpox. Ten employees have had contact with this patient. Those employees with significant exposure may be furloughed after exposure. "Significant exposure" is considered
greater than one hour of direct patient contact occurring within 24 hours prior to the appearance of lesions.
sharing the same air space for any duration of time after the patient has developed skin lesions.
unprotected contact with respiratory secretions or skin lesions occurring after 12 hours of the appearance of lesions.
irrelevant unless the employee has a negative varicella antibody titer.
Chickenpox (varicella) is primarily spread throughairborne transmission, and exposure is defined bybeing in the same airspacewith a contagious person (from 1-2 days before rash onset until lesions are crusted), even if briefly.
TheAPIC Textstates:
“Significant exposure is defined as being in the same room or airspace during the period of infectivity, regardless of duration”.
This reflects airborne precaution definitions and CDC exposure management guidelines for varicella.
Which of the following BEST demonstrates the effectiveness of a program targeted at reducing central-line associated bloodstream infections (CLABSIs) in an intensive care unit (ICU)?
A 25% decrease in the length of stay in the ICU related to CLABSIs
A 25% reduction in the incidence of CLABSIs over 6 months
A 30% decrease in total costs related to treatment of CLABSIs over 12 months
A 30% reduction in the use of antibiotic-impregnated central catheters over 6 months
Evaluating the effectiveness of a program to reduce central-line associated bloodstream infections (CLABSIs) in an intensive care unit (ICU) requires identifying the most direct and relevant measure of success. The Certification Board of Infection Control and Epidemiology (CBIC) emphasizes outcome-based assessment in the "Performance Improvement" and "Surveillance and Epidemiologic Investigation" domains, aligning with the Centers for Disease Control and Prevention (CDC) guidelines for infection prevention. The primary goal of a CLABSI reduction program is to decrease the occurrence of these infections, with secondary benefits including reduced length of stay, costs, and resource use.
Option B, "A 25% reduction in the incidence of CLABSIs over 6 months," is the best demonstration of effectiveness. The incidence of CLABSIs—defined by the CDC as the number of infections per 1,000 central line days—directly measures the program’s impact on the targeted outcome: preventing bloodstream infections associated with central lines. A 25% reduction over 6 months indicates a sustained decrease in infection rates, providing clear evidence that the intervention (e.g., improved insertion techniques, maintenance bundles, or staff education) is working. The CDC’s "Guidelines for the Prevention of Intravascular Catheter-Related Infections" (2017) and the National Healthcare Safety Network (NHSN) protocols prioritize infection rate reduction as the primary metric for assessing CLABSI prevention programs.
Option A, "A 25% decrease in the length of stay in the ICU related to CLABSIs," is a secondary benefit. Reducing CLABSI-related length of stay can improve patient outcomes and bed availability, but it is an indirect measure dependent on infection incidence. A decrease in length ofstay could also reflect other factors (e.g., improved discharge planning), making it less specific to program effectiveness. Option C, "A 30% decrease in total costs related to treatment of CLABSIs over 12 months," reflects a financial outcome, which is valuable for justifying resource allocation. However, cost reduction is a downstream effect of decreased infections and may be influenced by variables like hospital pricing or treatment protocols, diluting its direct link to program success. Option D, "A 30% reduction in the use of antibiotic-impregnated central catheters over 6 months," indicates a change in practice but not necessarily effectiveness. Antibiotic-impregnated catheters are one prevention strategy, and reducing their use could suggest improved standard practices (e.g., chlorhexidine bathing), but it could also increase infection rates if not offset by other measures, making it an ambiguous indicator.
The CBIC Practice Analysis (2022) and CDC guidelines emphasize that the primary measure of a CLABSI prevention program’s success is a reduction in infection incidence, as it directly addresses patient safety and the program’s core objective. Option B provides the most robust and specific evidence of effectiveness over a defined timeframe.

TESTED 17 Dec 2025
Copyright © 2014-2025 DumpsTool. All Rights Reserved
